Christopher C. Schmidt, MD, is a board-certified, fellowship-trained orthopedic shoulder and elbow surgeon who is nationally recognized for both his surgical acumen and groundbreaking research. At his state-of-the-art biomechanical lab in Pittsburgh, Pennsylvania, he performs extensive studies to continually enhance the understanding of shoulder and elbow injuries from both a clinical perspective and a research perspective. Dr. Schmidt has contributed to significant advancements in the diagnosis, treatment, and prevention of shoulder and elbow injuries, ultimately improving patient care through evidence-based medicine.
When Is a Surgical Repair Appropriate for a Distal Biceps Tendon Tear?
Widely regarded as an expert among experts, Dr. Schmidt is committed to keeping his fellow surgeons up to date on current best practices and emerging trends in his field, including the latest approaches for repairing distal biceps tendon tears.
In 2011, Dr. Schmidt was nominated for the prestigious Charles S. Neer Award given by the American Shoulder and Elbow Surgeons for his work on a study entitled “MRI Appearance of Distal Biceps Tendon and Comparison with Functional Outcome.” The objective of this study was to determine whether the MRI appearance of a repaired distal biceps tendon correlates to the clinical outcome. The findings suggest that clinical decisions for the reoperation of a painful distal biceps repair should not be solely based on the MRI appearance of the tendon.
Recently, Dr. Schmidt participated in an important research study to help his peers and patients determine when it is appropriate to surgically repair a partial distal biceps tendon rupture based on the extent and location of the tear. The abstract of this study, which is reproduced below, was submitted to the American Academy of Orthopaedic Surgeons (AAOS) and was accepted for a podium presentation at the annual meeting in Orlando, Florida.
Partial Distal Biceps Ruptures Results in a Substantial Loss of Supination Force
Tomizuka Y, Schmidt CC, Delserro S, Spicer C, Brown BT, Mauro RJ, Miller MC, Smolinski PJ
Shoulder and Elbow Mechanical Laboratory, University of Pittsburgh Medical Center, Pittsburgh, PA, U.S.A
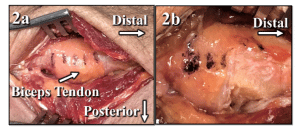
Methods: The mechanical tests performed measured isometric forearm supination moment arms in 60º of pronation, neutral, and 60º of supination and elbow flexion force using a validated anatomic elbow simulator, as previously published (3). Mechanical testing was performed on 18 adult fresh-frozen upper extremity cadaveric specimens (average age 57.3±13.2).
In the other 9 specimens, the biceps tendon was released and tested in a similar manner, but the tendon was released starting proximal (proximal-first). The starting cut sequence, distal- or proximal-first, was randomly assigned. Significance (p<0.05) was tested with a one-way ANOVA.
Results: In distal-first release specimens, the only significant decreases in supination moment arm occurred in the 75% release groups: 24% of intact state in 60º of pronation (p=0.003) and 10% in neutral (p=0.043). A 29% decrease occurred in 60º of supination (p=0.056).
In proximal-first release specimens there were no significant differences in supination moment arms for the 25%, 50%, and 75% releases in 60º of pronation, neutral, or 60º of supination forearm positions (p≥0.079).
No significant change occurred in the elbow flexion force by releasing the distal- or proximal-first 25%, 50%, or 75% of the biceps tendon (p≥0.058).
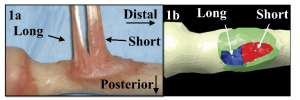
Discussion: Clinically, partial biceps ruptures usually involve all or a sizeable part of the short head attachment (2). This study clearly shows that a full short head rupture (distal-first 75% cut) can cause substantial disability because it results in a 24%, 10%, and 29% loss of supination moment arm (compared to native) in pronated, neutral, and supinated forearm positions, respectively.
A partial proximal-first release did not substantially change the supination moment arm implying the short head vs. long head is more important determinant of supination strength. Despite previous studies showing the short to be a better elbow flexor (1,4), a partial short head release (distal-first) did not change the elbow flexion force.
Clinical Significance: In a recent clinical series, an MRI-diagnosed partial tear >50% was a predictor of needing surgery (odds ratio 3.0, p=0.006) (5). This study supports this concept if the partial tear is distal. A >50% distal lesion would represent a near complete short head rupture; our findings clearly show that a complete short head lesion results in a significant loss of supination moment arm in pronated and neutral forearm positions (p≤0.043). A biomechanical case could be made for early repair of high-grade short head ruptures to optimally restore supination strength and improve ultimate function.
References: (1) JSES (2012) 21, 942-48. (2) JSES (2017) 26, 403-08. (3) JBJS (2015) 97-A 2014-23. (4) JBJS 2007 89, 1044-49(5) JSES (2018) 27, 720-25.
To learn more about the latest surgical treatment techniques for partial distal biceps tendon tears, contact Dr. Schmidt’s office today at (877) 471-0935 to schedule an appointment.